Quality metric to assess adequacy of hydrogel rectal spacer placement for prostate radiation therapy and association of metric score with rectal toxicity outcomes Journal Article
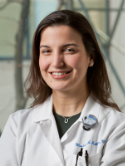
| Authors: | Grossman, C. E.; Folkert, M. R.; Lobaugh, S.; Desai, N. B.; Kollmeier, M. A.; Gorovets, D.; McBride, S. M.; Timmerman, R. D.; Zhang, Z.; Zelefsky, M. J. |
| Article Title: | Quality metric to assess adequacy of hydrogel rectal spacer placement for prostate radiation therapy and association of metric score with rectal toxicity outcomes |
| Abstract: | Purpose: Although hydrogel spacer placement (HSP) minimizes rectal dose during prostate cancer radiation therapy, its potential benefit for modulating rectal toxicity could depend on the achieved prostate-rectal separation. We therefore developed a quality metric associated with rectal dose reduction and late rectal toxicity among patients treated with prostate stereotactic body radiation therapy (SBRT). Methods and Materials: A quality metric consisting of prostate-rectal interspace measurements from axial T2-weighted magnetic resonance imaging simulation images was applied to 42 men enrolled in a multi-institutional phase 2 study using HSP with prostate SBRT (45 Gy in 5 fractions). A score of 0, 1, or 2 was assigned to a prostate-rectal interspace measurement of <0.3 cm, 0.3 to 0.9 cm, or ≥1 cm, respectively. An overall spacer quality score (SQS) was computed from individual scores at rectal midline and ±1 cm laterally, located at the prostate base, midgland, and apex. Associations of SQS with rectal dosimetry and late toxicity were evaluated. Results: The majority of the analyzed cohort had an SQS of 1 (n = 17; 41%) or 2 (n = 18; 43%). SQS was associated with maximum rectal point dose (rectal Dmax; P = .002), maximum dose to 1 cc of rectum (D1cc; P = .004), and volume of rectum receiving ≥100% of prescription dose (V45; P = .046) and ≥40 Gy (V40; P = .005). SQS was also associated with a higher incidence of (P = .01) and highest-graded late rectal toxicity (P = .01). Among the 20 men who developed late grade ≥1 rectal toxicity, 57%, 71%, and 22% had an SQS of 0, 1, and 2, respectively. Men with an SQS of 0 or 1 compared with 2 had 4.67-fold (95% CI, 0.72-30.11) or 8.40-fold (95% CI, 1.83-38.57) greater odds, respectively, of developing late rectal toxicity. Conclusions: We developed a reliable and informative metric for assessing HSP, which appears to be associated with rectal dosimetry and late rectal toxicity after prostate SBRT. © 2022 |
| Keywords: | adult; clinical article; controlled study; treatment planning; comparative study; nuclear magnetic resonance imaging; outcome assessment; follow up; disease association; phase 2 clinical trial; cohort analysis; prostate cancer; health insurance; multicenter study; seminal vesicle; toxicity; stereotactic body radiation therapy; secondary analysis; rectum injury; maximum permissible dose; hydrogel; human; male; article; t2 weighted imaging; american urological association symptom index |
| Journal Title: | Advances in Radiation Oncology |
| Volume: | 8 |
| Issue: | 4 |
| ISSN: | 2452-1094 |
| Publisher: | Elsevier Inc. |
| Date Published: | 2023-07-01 |
| Start Page: | 101070 |
| Language: | English |
| DOI: | 10.1016/j.adro.2022.101070 |
| PROVIDER: | scopus |
| PMCID: | PMC10196227 |
| PUBMED: | 37213478 |
| DOI/URL: | |
| Notes: | Article -- Source: Scopus |
Altmetric
Citation Impact
BMJ Impact Analytics
Related MSK Work