Early quality of life outcomes after robotic-assisted minimally invasive and open esophagectomy Journal Article
| Authors: | Sarkaria, I. S.; Rizk, N. P.; Goldman, D. A.; Sima, C.; Tan, K. S.; Bains, M. S.; Adusumilli, P. S.; Molena, D.; Bott, M.; Atkinson, T.; Jones, D. R.; Rusch, V. W. |
| Article Title: | Early quality of life outcomes after robotic-assisted minimally invasive and open esophagectomy |
| Abstract: | Background: Minimally invasive esophagectomy may improve some perioperative outcomes over open approaches; effects on quality of life are less clear. Methods: A prospective trial of robotic-assisted minimally invasive esophagectomy (RAMIE) and open esophagectomy was initiated, measuring quality of life via the Functional Assessment of Cancer Therapy–Esophageal and Brief Pain Inventory. Mixed generalized linear models assessed associations between quality of life scores over time and by surgery type. Results: In total, 106 patients underwent open esophagectomy; 64 underwent minimally invasive esophagectomy (98% RAMIE). The groups did not differ in age, sex, comorbidities, histologic subtype, stage, or induction treatment (P =.42 to P >.95). Total Functional Assessment of Cancer Therapy–Esophageal scores were lower at 1 month (P <.001), returned to near baseline by 4 months, and did not differ between groups (P =.83). Brief Pain Inventory average pain severity (P =.007) and interference (P =.004) were lower for RAMIE. RAMIE had lower estimated blood loss (250 vs 350 cm3; P <.001), shorter length of stay (9 vs 11 days; P <.001), fewer intensive care unit admissions (8% vs 20%; P =.033), more lymph nodes harvested (25 vs 22; P =.05), and longer surgical time (6.4 vs 5.4 hours; P <.001). Major complications (39% for RAMIE vs 52% for open esophagectomy; P >.95), anastomotic leak (3% vs 9%; P =.41), and 90-day mortality (2% vs 4%; P =.85) did not differ between groups. Pulmonary (14% vs 34%; P =.014) and infectious (17% vs 36%; P =.029) complications were lower for RAMIE. Conclusions: RAMIE is associated with lower immediate postoperative pain severity and interference and decreased pulmonary and infectious complications. Ongoing data accrual will assess mid-term and long-term outcomes in this cohort. © 2019 The Society of Thoracic Surgeons |
| Journal Title: | Annals of Thoracic Surgery |
| Volume: | 108 |
| Issue: | 3 |
| ISSN: | 0003-4975 |
| Publisher: | Elsevier Science, Inc. |
| Date Published: | 2019-01-01 |
| Start Page: | 920 |
| End Page: | 928 |
| Language: | English |
| DOI: | 10.1016/j.athoracsur.2018.11.075 |
| PUBMED: | 31026433 |
| PROVIDER: | scopus |
| PMCID: | PMC6774254 |
| DOI/URL: | |
| Notes: | Article -- Export Date: 4 September 2019 -- Source: Scopus |
Altmetric
Citation Impact
BMJ Impact Analytics
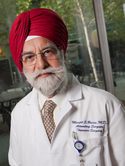
MSK Authors
Related MSK Work