Chest wall resection and reconstruction for T4 non-small cell lung cancer Editorial
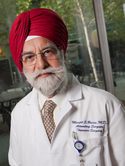
| Authors: | Caso, R.; Sutton, W.; Bains, M. S.; Shahzad, F.; Jones, D. R.; Rocco, G. |
| Title: | Chest wall resection and reconstruction for T4 non-small cell lung cancer |
| Abstract: | Chest wall resection and reconstruction for T4 non-small cell lung cancer (NSCLC) represents a challenging surgical scenario; T4 Pancoast tumors and tumors involving the spine (T4 spine) are the most frequently encountered subsets. Multidisciplinary assessment is performed to select the optimal surgical approach, determine the extent of resection necessary to obtain tumor-free margins, define the geometric characteristics of the chest wall defect, and choose the most appropriate reconstructive materials. Two or 3 incisions, selected on the basis of the individual patient, are recommended to access T4 Pancoast tumors. Depending on the level of involvement of the vertebral structure, the approach to the T4 spine may require a thoracotomy and a midline posterior incision. Chest wall reconstruction is often complicated by sequelae of chemoradiation or chemoimmunotherapy, superimposed infection, or anatomic derangement after previous surgery. Since 2019, the Chest Wall Multidisciplinary Team at Memorial Sloan Kettering Cancer Center has generated several recommendations for chest wall resection and reconstruction for patients with T4 tumors. Anterior defects are generally reconstructed using rigid materials. T4 Pancoast tumors are preferentially reconstructed using semirigid (biologic) materials and a bulky free flap, which provide similar stability as rigid materials and avoid impingement on the thoracic inlet neurovascular bundle. For posterior defects, semirigid resorbable materials are used to avoid pleural fluid extravasation and seromas. The use of free flaps allows more-extensive chest wall resection and promises a high likelihood of R0 resection, with morbidity similar to that with regional flaps. A multidisciplinary approach ensures optimal management of these complex cases. © 2025 Elsevier Inc. |
| Keywords: | spine tumors; pancoast tumors; chest wall reconstruction; t4 lung cancer |
| Journal Title: | Seminars in Thoracic and Cardiovascular Surgery |
| ISSN: | 1043-0679 |
| Publisher: | Elsevier Inc. |
| Publication status: | Online ahead of print |
| Date Published: | 2025-07-02 |
| Online Publication Date: | 2025-07-02 |
| Language: | English |
| DOI: | 10.1053/j.semtcvs.2025.05.012 |
| PUBMED: | 40614793 |
| PROVIDER: | scopus |
| DOI/URL: | |
| Notes: | Source: Scopus |
Altmetric
Citation Impact
BMJ Impact Analytics
Related MSK Work