Does the SORG algorithm generalize to a contemporary cohort of patients with spinal metastases on external validation? Journal Article
| Authors: | Bongers, M. E. R.; Karhade, A. V.; Villavieja, J.; Groot, O. Q.; Bilsky, M. H.; Laufer, I.; Schwab, J. H. |
| Article Title: | Does the SORG algorithm generalize to a contemporary cohort of patients with spinal metastases on external validation? |
| Abstract: | BACKGROUND CONTEXT: The SORG machine-learning algorithms were previously developed for preoperative prediction of overall survival in spinal metastatic disease. On sub-group analysis of a previous external validation, these algorithms were found to have diminished performance on patients treated after 2010. PURPOSE: The purpose of this study was to assess the performance of these algorithms on a large contemporary cohort of consecutive spinal metastatic disease patients. STUDY DESIGN/SETTING: Retrospective study performed at a tertiary care referral center. PATIENT SAMPLE: Patients of 18 years and older treated with surgery for metastatic spinal disease between 2014 and 2016. OUTCOME MEASURES: Ninety-day and one-year mortality. METHODS: Baseline patient and tumor characteristics of the validation cohort were compared to the development cohort using bivariate logistic regression. Performance of the SORG algorithms on external validation in the contemporary cohort was assessed with discrimination (c-statistic and receiver operating curve), calibration (calibration plot, intercept, and slope), overall performance (Brier score compared to the null-model Brier score), and decision curve analysis. RESULTS: Overall, 200 patients were included with 90-day and 1-year mortality rates of 55 (27.6%) and 124 (62.9%), respectively. The contemporary external validation cohort and the developmental cohort differed significantly on primary tumor histology, presence of visceral metastases, American Spinal Injury Association impairment scale, and preoperative laboratory values. The SORG algorithms for 90-day and 1-year mortality retained good discriminative ability (c-statistic of 0.81 [95% confidence interval [CI], 0.74–0.87] and 0.84 [95% CI, 0.77–0.89]), overall performance, and decision curve analysis. The algorithm for 90-day mortality showed almost perfect calibration reflected in an overall calibration intercept of −0.07 (95% CI: −0.50, 0.35). The 1-year mortality algorithm underestimated mortality mainly for the lowest predicted probabilities with an overall intercept of 0.57 (95% CI: 0.18, 0.96). CONCLUSIONS: The SORG algorithms for survival in spinal metastatic disease generalized well to a contemporary cohort of consecutively treated patients from an external institutional. Further validation in international cohorts and large, prospective multi-institutional trials is required to confirm or refute the findings presented here. The open-access algorithms are available here: https://sorg-apps.shinyapps.io/spinemetssurvival/. © 2020 Elsevier Inc. |
| Keywords: | adult; cancer survival; aged; survival analysis; cancer surgery; primary tumor; major clinical study; histopathology; mortality; cancer patient; comparative study; outcome assessment; preoperative evaluation; sensitivity and specificity; quality control; calibration; cohort analysis; validation study; retrospective study; prediction; algorithm; laboratory test; visceral metastasis; predictive value; spine metastasis; hospital mortality; spinal metastases; metastasis resection; external validation; prognostication; mortality rate; machine learning; normal value; cancer prognosis; human; male; female; priority journal; article; tertiary care center; prognostic assessment; american spinal injury association impairment scale; mortality risk score; sorg algorithm |
| Journal Title: | Spine Journal |
| Volume: | 20 |
| Issue: | 10 |
| ISSN: | 1529-9430 |
| Publisher: | Elsevier Science Inc. |
| Date Published: | 2020-10-01 |
| Start Page: | 1646 |
| End Page: | 1652 |
| Language: | English |
| DOI: | 10.1016/j.spinee.2020.05.003 |
| PUBMED: | 32428674 |
| PROVIDER: | scopus |
| DOI/URL: | |
| Notes: | Article -- Export Date: 2 November 2020 -- Source: Scopus |
Altmetric
Citation Impact
BMJ Impact Analytics
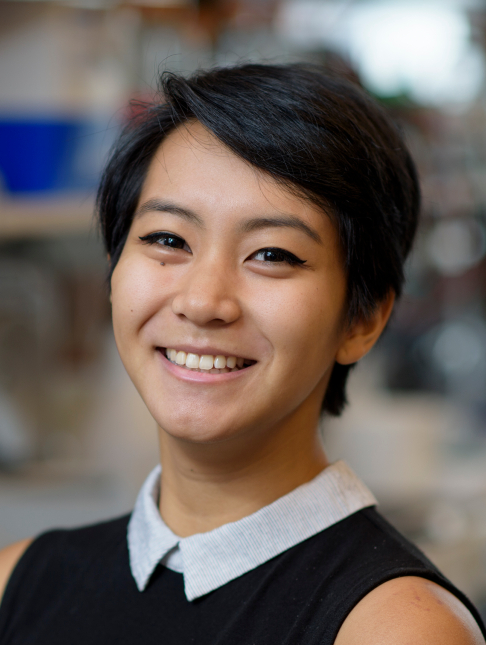
MSK Authors
Related MSK Work